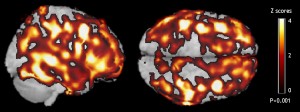
Two views of a composite image of the brains analyzed in Dr. Mosconi’s study highlight the average increase in amyloid-beta deposits among 14 healthy adults with a mother affected by Alzheimer’s. Regions in yellow have 4 times more amyloid than the corresponding regions of 14 healthy counterparts with no family history of dementia, while regions in red have twice as much amyloid.
New imaging tool could eventually lead to earlier detection among pre-symptomatic individuals
A family history of Alzheimer’s is one of the biggest risk factors for developing the memory-robbing disease, which affects more than 5 million Americans and is the most common form of senile dementia. Now an international collaboration led by NYU Langone Medical Center researchers has found the likely basis for this heightened familial risk—especially from the maternal side.
Aided by a new version of a brain scanning technique, the researchers discovered a far greater number of protein clumps linked to the disease among healthy adult children of parents with Alzheimer’s compared to counterparts with no family history of dementia. The average increase in these clumps, called amyloid-beta plaques, was particularly striking among study volunteers whose mothers had been diagnosed with the disease. The plaques appeared throughout most regions of the brain.
The study examined 42 healthy individuals, including 14 whose mothers had Alzheimer’s, 14 whose fathers had Alzheimer’s, and 14 counterparts with no family history of the disease. On average, the first group of volunteers showed a 15 percent higher burden of amyloid-beta deposits than those with a paternal family history, and a 20 percent higher burden of the protein clumps than those with no familial risk factors.
The new findings, published in the March 15, 2010, online early edition of Proceedings of the National Academy of Sciences, may help explain why a family history is such a big risk factor for the brain disease—individuals with an affected parent have a four- to ten-fold greater risk than those with no family history.
The study was led by Lisa Mosconi, PhD, research assistant professor of psychiatry at NYU Langone, and colleagues at NYU Langone who collaborated with researchers at the University of Turku in Finland and Weill Cornell Medical Center in New York.
“Given that brain pathology begins to accumulate years ahead of memory problems in Alzheimer’s disease, our findings are intriguing,” says Dr. Mosconi. “There is a great effort underway to find early markers of disease, before symptoms appear, so that therapeutic approaches will one day delay or ultimately prevent this disease.”
Amyloid plaques are one of the hallmarks of Alzheimer’s disease, although not everyone with plaques develops the disease. For many years, amyloid-beta plaques could only be measured in autopsied brains, but methods have recently emerged that allow the plaques to be observed in living brains.
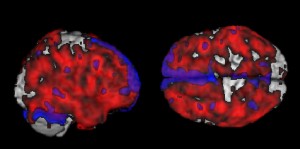
The new study combines positron emission tomography (PET) with a fluorescent dye called Pittsburgh Compound B (PiB) that highlights brain amyloid plaques, enabling researchers to actually see the deposits. The dye attaches to plaques and acts like a temporary beacon to highlight their presence during a PET scan. Dr. Mosconi cautions that her team’s imaging technique is a potentially powerful research tool and is not ready for use as a diagnostic tool in the clinic.
Plaques begin forming in the brain when, for unknown reasons, normal amyloid-beta proteins change their shape and structure and begin sticking together. The presence of plaques, however, does not necessarily mean an individual will develop Alzheimer’s, and much of the harm may arrive well before the plaques appear—no one can yet say whether they are a cause or a consequence of the disease.
It isn’t known why the deposits were more common among children of parents with the disease in the study, but Dr. Mosconi suspects that a genetic mechanism is involved. “At this point, we can only speculate that genes that are transmitted from parents, particularly mothers, to their children lead to amyloid depositions, which increase risk for developing dementia,” she says.
Dr. Mosconi and her colleagues hope to follow the study’s 42 volunteers and more subjects over time to analyze the link between plaque formation and Alzheimer’s. For those who never develop dementia, she likewise hopes to determine what preventive factors may be neutralizing the bad effects of amyloid on the brain.
The scanning technique used in the new study also provides more evidence supporting a maternal family link to Alzheimer’s, notes Dr. Mosconi, whose previous studies have shown such an association based on reduced glucose metabolism in the brains of healthy adults whose mothers had the disease.
“This imaging study further anchors the risk for Alzheimer’s disease associated with having a mother affected by the disease,” says Mony J. de Leon, EdD, professor of psychiatry and Director of the Center for Brain Health at NYU Langone Medical Center, and one of the study’s authors.
The study’s co-authors include Yi Li, Huiyu Wang, John Murray, Schantel Williams, Lidia Glodzik, Wai Tsui and Susan De Santi from NYU Langone Medical Center; Juha Rinne and Noora Scheinin from the University of Turku; Kjell NÃ¥gren from Turku and Odense University Hospital, Denmark; and Shankar Vallabhajosula from Weill Cornell Medical College.
The study was supported by grants from the National Institutes of Health’s National Institute on Aging and National Center for Research Resources, the Alzheimer’s Association, the Academy of Finland, the Sigrid Juselius Foundation, and Turku University Hospital.
Source: New York University Langone Medical Center
