 While antidepressant medications have proven to be beneficial in helping people overcome major depression, it has long been known that a small subset of individuals taking these drugs can actually experience a worsening of mood, and even thoughts of suicide. No clinical test currently exists to make this determination, and only time — usually weeks — can tell before a psychiatrist knows whether a patient is getting better or worse.
While antidepressant medications have proven to be beneficial in helping people overcome major depression, it has long been known that a small subset of individuals taking these drugs can actually experience a worsening of mood, and even thoughts of suicide. No clinical test currently exists to make this determination, and only time — usually weeks — can tell before a psychiatrist knows whether a patient is getting better or worse.
Now, UCLA researchers have developed a non-invasive biomarker, or indicator, that may serve as a type of early warning system.
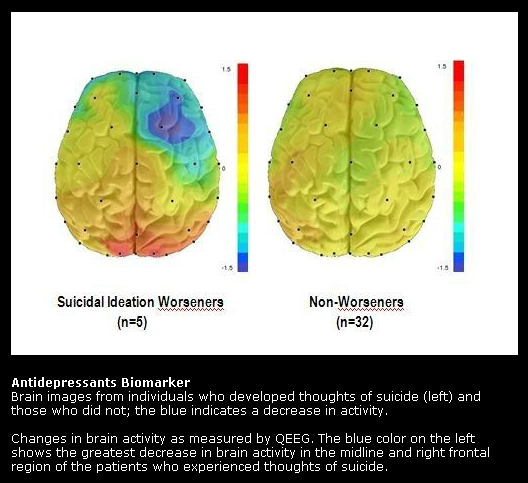
Reporting in the April edition of the peer-reviewed journal Acta Psychiatrica Scandinavica, Aimee Hunter, an assistant research psychologist in the UCLA Department of Psychiatry, and colleagues report that by using quantitative electroencephalographic (QEEG), a non-invasive measurement of electrical activity in the brain, they were able to observe a sharp reduction of activity in a specific brain region in individuals who proved susceptible to thoughts of suicide — within 48 hours of the start of treatment.
Prior research, Hunter said, has shown that between 8 and 14 percent of depressed patients develop thoughts of suicide while taking the most common forms of depression drugs, known as selective serotonin reuptake inhibitors (SSRI). Although reports have suggested that SSRIs are to blame, no firm link between these drugs and thoughts of suicide has been established.
This study suggests, for the first time, a link between worsening suicidality and specific changes in brain function while on these medications.
The researchers treated 72 people suffering from major depressive disorder (MDD) with one of two antidepressants, fluoxetine or venlafaxine, or with a placebo. All were evaluated by a clinician using the Hamilton Depression Rating Scale, a standard instrument that assesses the severity of a wide range of depression symptoms. Of the 37 participants on medication, five (13.5 percent) had worsening thoughts of suicide.
All of the participants were also examined using QEEG, which evaluates brain function based on the brain’s electrical activity. Among the 13.5 percent of participants who got worse, the researchers found a sharp drop in brain activity within 48 hours of the start of medication. The drop occurred in the midline and right-frontal sections of the brain, areas known to control emotions.
Of note, eight of the 35 participants taking a placebo (22.9 percent) also had increased thoughts of suicide. However, the placebo participants did not show the precipitous drop in brain activity within the first 48 hours.
“This is the first study to show a change in brain function after the start of medication that appears to be linked to the subsequent development of worsening thoughts of suicide during antidepressant treatment,” Hunter said. “Importantly, changes in this biomarker did not predict worsening suicidal thoughts in the placebo-treated subjects, so the results suggest that the biomarker specifically detected medication-related worsening only.”
QEEG is a relatively inexpensive instrument that is non-invasive; measurements are obtained by placing electrodes on the scalp. As a result, Hunter said, further development of this biomarker could potentially lead to a tool that could be used by clinicians to predict, in the early stages of treatment, whether an individual suffering from depression will develop thoughts of suicide.
Other authors of the study included Andrew Leuchter, Ian Cook and Michele Abrams, all of UCLA.
Funding for the study was provided by the National Institute of Mental Health; the National Center for Complementary and Alternative Medicine; grants from Lilly Research Laboratories, Wyeth Pharmaceuticals and Aspect Medical Systems; and an endowment from Joanne and George Miller and family to the UCLA Brain Research Institute. The funding providers had no role in any aspect of the study.
Source: UCLA
