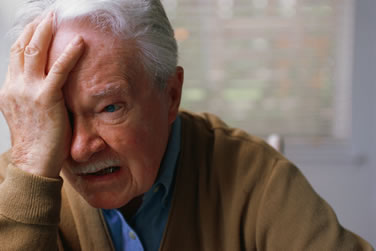
Depression in the elderly is frequently unrecognized by physicians. This study attempts to understand why. Studies that examined the unassisted (clinical) ability of general practitioners (GPs; primary care physicians) to identify depression were divided into those of older adults, younger adults and mixed populations.
Data were extracted by 3 reviewers independently and pooled using a Bayesian meta-analysis. 31 valid studies that examined both sensitivity and specificity (or rule-in and rule-out accuracy) were identified, involving 52,513 individuals. Twelve studies recruited older individuals, 12 recruited younger adults and 7 recruited both younger and older adults (mixed populations). In the most robust studies the point prevalence of depression in late life was 13.2% (95% CI = 7.9–19.6). GPs were able to correctly identify 47.3% of the late-life depressions and 78.6% of the non-cases (71.0% overall accuracy).
In younger adults GPs were able to identify 39.7% of the mid-life depressions and 85.1% of the non-depressed (77.8% overall accuracy). In mixed aged groups GPs were able to correctly identify 46.6% of the depressed individuals and 86.2% of the non-depressed (79.6% overall accuracy). The overall fraction correctly identified was significantly lower in older compared with younger adults. Correcting for differences in prevalence showed a statistically lower rule-in performance for older compared with younger adults.
There was no difference in ability to identify non-depressed (healthy) individuals by age. In clinical practice GPs appear to be less successful in identifying depression in older people than in younger adults, however there have been few head-to-head studies stratified by age from one centre.
Source: Journal of Psychotherapy and Psychosomatics :Mitchell, A.J. ; Rao, S. ; Vaze, A. Do Primary Care Physicians Have Particular Difficulty Identifying Late-Life Depression? A Meta-Analysis Stratified by Age. Psychother Psychosom 2010;79:285-294